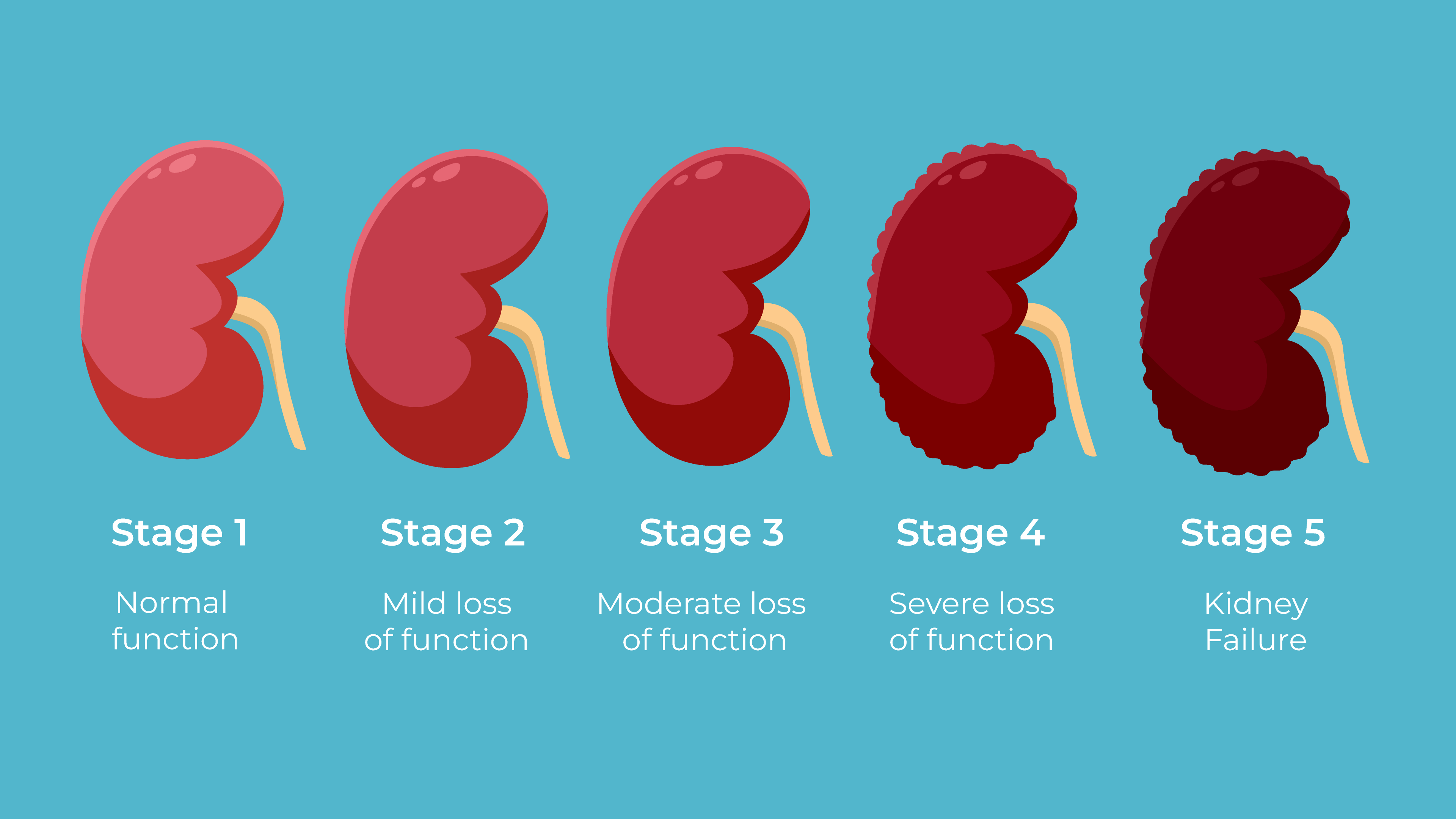
Kidney disease is a condition that worsens over time, leading to significant impacts on health and life expectancy. There are five stages of kidney disease, each representing a further decline in kidney function.
As the disease progresses from mild damage in the early stages to complete kidney failure in the final stage, the risks and challenges increase. Understanding what each stage entails can help in managing the disease more effectively.
This article will guide you through the five stages of kidney disease, explaining how each stage affects your health and what it means for your life expectancy.
Table of Contents
ToggleThese are the 5 Stages of Kidney Disease
- Stage 1: Kidney function is normal, but there are signs of mild damage
- Stage 2: Mild loss of kidney function with a decrease in eGFR
- Stage 3: Moderate loss of kidney function, with further reduction in eGFR, split into 3a and 3b
- Stage 4: Severe reduction in kidney function, eGFR drops significantly, leading to more serious health complications
- Stage 5: Kidney failure, eGFR is less than 15, requiring dialysis or a kidney transplant
Stage 1: Kidney Function is Normal, but There are Signs of Mild Damage
| Stage | eGFR (mL/min/1.73m²) | Key Characteristics | Symptoms | Management |
|---|---|---|---|---|
| Stage 1 | 90 or higher | Kidney function is normal with mild signs of damage, such as protein in the urine | Often asymptomatic or subtle signs like high blood pressure | Regular monitoring, managing blood pressure, healthy lifestyle changes |
In Stage 1 Chronic Kidney Disease, kidney function is still normal, with an eGFR of 90 or higher. However, early signs of kidney damage are present, such as protein in the urine, also known as albuminuria. This stage often lacks noticeable symptoms, making it easy for the condition to go undetected unless identified through routine tests.
According to the National Kidney Foundation, it is crucial to identify CKD in its early stages to slow progression and prevent further damage. Dr. Joseph Vassalotti, Chief Medical Officer of the National Kidney Foundation, emphasizes that early detection allows for interventions that can maintain kidney function longer.
Management
At this stage, the primary focus is on monitoring and managing any underlying conditions that could contribute to further kidney damage, such as hypertension or diabetes. Regular check-ups, a balanced diet low in sodium, and maintaining a healthy lifestyle are recommended to slow disease progression.
It is also important to avoid medications that could harm the kidneys, such as NSAIDs.
Stage 2: Mild Loss of Kidney Function with a Decrease in eGFR
| Stage | eGFR (mL/min/1.73m²) | Key Characteristics | Symptoms | Management |
|---|---|---|---|---|
| Stage 2 | 60-89 | Mild loss of kidney function, with early signs of kidney damage | Often asymptomatic, possible high blood pressure, slight changes in urine composition | Regular monitoring, blood pressure management, lifestyle changes, dietary adjustments |
In Stage 2 Chronic Kidney Disease, there is a mild reduction in kidney function, with an eGFR between 60 and 89. Kidney damage is more apparent than in Stage 1, often detected through increased levels of protein in the urine or other abnormalities. Although the kidneys are still functioning relatively well, early intervention is essential to slow the progression of the disease.
Dr. Andrew Narva, a nephrologist with extensive experience in kidney disease, highlights the importance of addressing any underlying health issues at this stage. “Even though the decline in kidney function might seem mild, it is a critical period for implementing changes that can have a long-term impact on health outcomes,” says Dr. Narva.
Management
The management of Stage 2 CKD focuses on preventing further kidney damage through regular monitoring, blood pressure control, and lifestyle modifications. This includes adopting a diet low in salt and protein, managing blood sugar levels in diabetic patients, and ensuring regular physical activity.
Patients are advised to avoid nephrotoxic medications and to consult with a healthcare provider before taking any new drugs.
Stage 3: Moderate Loss of Kidney Function
| Stage | eGFR (mL/min/1.73m²) | Key Characteristics | Symptoms | Management |
|---|---|---|---|---|
| Stage 3a | 45-59 | Mild to moderate loss of kidney function | Swelling, fatigue, changes in urination, back pain | Regular check-ups, kidney-friendly diet, medications to manage complications |
| Stage 3b | 30-44 | Moderate to severe loss of kidney function | More pronounced symptoms, including uremia | Referral to nephrologist, managing underlying conditions, possibly preparing for dialysis |
Stage 3 Chronic Kidney Disease signifies a moderate decline in kidney function, with an eGFR between 30 and 59. At this stage, kidney damage is significant enough that many individuals begin to experience noticeable symptoms, such as swelling in the extremities, fatigue, and changes in urination. Early detection and management are critical to slowing the progression of the disease.
Dr. Michael J. Choi, Director of the Division of Nephrology at MedStar Georgetown University Hospital, highlights the critical need for early intervention in Stage 3 CKD. “Patients should focus on controlling blood pressure and blood sugar levels, as these are key factors in slowing the progression of kidney disease,” Dr. Choi advises.
He also emphasizes the importance of dietary changes and regular monitoring to prevent further kidney damage.
Management
Management of Stage 3 CKD includes regular monitoring of kidney function, dietary modifications to limit intake of sodium, protein, and phosphorus, and addressing any underlying conditions. Medications such as ACE inhibitors or ARBs may be prescribed to help protect kidney function and control blood pressure.
Patients are also advised to avoid nephrotoxic medications and to consult with their healthcare providers before taking any new medications.
Stage 4: Severe Loss of Kidney Function
| Stage | eGFR (mL/min/1.73m²) | Key Characteristics | Symptoms | Management |
|---|---|---|---|---|
| Stage 4 | 15-29 | Severe loss of kidney function | Significant symptoms such as fatigue, swelling, and changes in urination | Planning for dialysis or transplant, managing symptoms, dietary changes |
Stage 4 Chronic Kidney Disease represents a severe decline in kidney function, with an eGFR between 15 and 29. At this stage, the kidneys are heavily damaged and are no longer able to filter waste and excess fluids effectively.
As a result, symptoms become more pronounced, and there is a heightened risk of complications such as anemia, bone disease, and cardiovascular issues. This stage is critical for preparing for potential kidney failure and considering treatment options such as dialysis or a kidney transplant.
Dr. Jamin Brahmbhatt, a urologist and expert in chronic kidney disease, emphasizes the importance of comprehensive care during Stage 4 CKD. “Patients at this stage must be closely monitored and managed with a multidisciplinary approach to slow the disease’s progression and manage symptoms effectively.
Preparing for treatments like dialysis or transplant becomes essential,” says Dr. Brahmbhatt. He also notes that lifestyle changes, such as adhering to a kidney-friendly diet and avoiding nephrotoxic medications, are crucial during this stage.
Management
Management of Stage 4 CKD involves more intensive medical care, including regular visits to a nephrologist. Patients are typically advised to follow a strict diet low in protein, sodium, potassium, and phosphorus to manage symptoms and prevent further kidney damage.
Medications to control blood pressure, blood sugar, and other underlying conditions are often necessary. Planning for dialysis or a kidney transplant becomes a priority, and patients are encouraged to discuss their options with their healthcare team to choose the best course of action.
Stage 5: Kidney Failure (End Stage Renal Disease)
| Stage | eGFR (mL/min/1.73m²) | Key Characteristics | Symptoms | Management |
|---|---|---|---|---|
| Stage 5 | Less than 15 | Kidney failure, requiring dialysis or transplant | Severe symptoms including fatigue, nausea, little to no urine production | Dialysis, kidney transplant, palliative care |
Stage 5 Chronic Kidney Disease, also known as end-stage renal disease (ESRD), is the final stage of kidney disease. At this point, the kidneys have lost nearly all their ability to function, with an eGFR of less than 15.
Without treatment, toxins and fluids build up in the body, leading to life-threatening complications. This stage requires immediate intervention, usually in the form of dialysis or a kidney transplant, to sustain life.
Dr. Steven Coca, a nephrologist at the Icahn School of Medicine at Mount Sinai, emphasizes the gravity of reaching Stage 5 CKD: “At this stage, the kidneys are no longer able to filter waste and excess fluids from the blood.
Patients must begin dialysis or undergo a kidney transplant to survive.” He adds that lifestyle modifications, while important, are no longer sufficient on their own, and medical treatment becomes the primary focus.
FAQs
What are the early signs of kidney disease?
Early signs of kidney disease can be subtle and may include symptoms like fatigue, difficulty concentrating, trouble sleeping, dry and itchy skin, and changes in urination patterns. In the early stages, symptoms are often mild or even absent, making it crucial to get regular check-ups if you have risk factors like high blood pressure, diabetes, or a family history of kidney disease.
Can kidney disease be reversed in its early stages?
Kidney disease cannot typically be reversed, but early detection and management can slow its progression. Lifestyle changes, such as adopting a kidney-friendly diet, controlling blood pressure, and managing blood sugar levels, can help preserve kidney function and prevent the disease from advancing to more severe stages.
What foods should be avoided if you have chronic kidney disease?
If you have chronic kidney disease, it’s important to limit foods high in sodium, potassium, and phosphorus. These include processed foods, certain fruits and vegetables like bananas and tomatoes, dairy products, and whole grains. A dietitian can help create a personalized meal plan that meets your nutritional needs while protecting your kidney function.
How does chronic kidney disease affect life expectancy?
The impact of chronic kidney disease on life expectancy varies depending on the stage at diagnosis, age, overall health, and how well the disease is managed. For example, individuals diagnosed with Stage 3 CKD may live for many years with proper treatment, while those in Stage 5 CKD often require dialysis or a kidney transplant to survive.
What happens if you refuse dialysis?
Refusing dialysis when it’s medically necessary, especially in Stage 5 CKD, typically leads to a rapid decline in health due to the buildup of toxins and fluids in the body. This can result in severe symptoms like swelling, shortness of breath, fatigue, and eventually, death. Patients should discuss their options thoroughly with their healthcare provider to make an informed decision.
Can chronic kidney disease cause other health problems?
Yes, chronic kidney disease can lead to various complications, including high blood pressure, anemia, bone disease, cardiovascular issues, and electrolyte imbalances. These complications arise because the kidneys are no longer able to perform their essential functions, like filtering waste and regulating essential minerals in the body. Regular monitoring and treatment are necessary to manage these risks.
Last Words
Chronic kidney disease is a serious condition that progressively worsens over time, affecting millions of people globally. Early detection and proper management can significantly slow the progression, especially in the initial stages.
However, as the disease advances to stages 4 and 5, more intensive treatments like dialysis or kidney transplantation become necessary to sustain life. It’s essential for individuals with CKD to work closely with their healthcare providers, adopt lifestyle changes, and stay informed about their treatment options to maintain the best possible quality of life.
Related Posts:
- COPD Life Expectancy - What Each of the 4 Stages Means?
- Seniors and Emergencies - The Five-Minute Rule That…
- How Music and Art Can Improve Daily Life for Seniors…
- Is Senior Life Insurance Company a Pyramid Scheme?…
- Pacemaker Surgery Recovery in the Elderly - What to…
- How Much Does a Living Trust Cost in the U.S. - Tips…