Abbreviations are a critical part of communication and documentation. They allow professionals to convey complex information quickly and efficiently. However, understanding these abbreviations is essential for both practitioners and patients to ensure accurate treatment and care.
This article explores the most frequently used abbreviations in physical therapy.
Table of Contents
ToggleList of Common Abbreviations in Physical Therapy
- Range of Motion (ROM)
- Fracture (Fx)
- Non-Weight Bearing (NWB)
- Full Weight-Bearing (FWB)
- Home Exercise Program (HEP)
- Physical Therapy (PT)
- Passive Range of Motion (PROM)
- Active Range of Motion (AROM)
- Transcutaneous Electrical Nerve Stimulation (TENS)
- Activities of Daily Living (ADL)
1. Range of Motion (ROM)
Range of Motion (ROM) refers to the measurement of the movement around a specific joint or body part. It is crucial in physical therapy as it helps therapists assess the flexibility, strength, and function of a patient’s joints.
ROM is typically measured in degrees and is divided into two main types: Passive Range of Motion (PROM) and Active Range of Motion (AROM).
- PROM involves the therapist moving the patient’s joint through its range without any effort from the patient. This is often used when the patient cannot move the joint on their own due to pain, weakness, or paralysis.
- AROM occurs when the patient actively uses their muscles to move the joint through its range. This type of movement is important for evaluating the functional capacity of the joint and muscles.
ROM is measured using a goniometer, a tool that allows therapists to accurately gauge the angle of the joint. Regular assessments of ROM are vital in tracking a patient’s progress during rehabilitation and ensuring that they regain as much mobility as possible after an injury or surgery. Factors such as age, gender, and physical condition can influence a person’s ROM, and physical therapy aims to maximize this range to restore normal function.
2. Fracture (Fx)
In physical therapy, a fracture, abbreviated as Fx, refers to a break in the continuity of a bone. Fractures can range from minor cracks to severe breaks that disrupt the structural integrity of the bone. The type and severity of the fracture dictate the treatment approach, which often involves immobilization, realignment, and rehabilitation.
Fractures are categorized based on their nature and location:
- Simple Fracture: A clean break with no damage to surrounding tissues or skin.
- Compound Fracture: The bone breaks through the skin, increasing the risk of infection.
- Comminuted Fracture: The bone is shattered into several pieces, often requiring surgical intervention.
- Stress Fracture: A small crack in the bone caused by repetitive force, common in athletes.
- Pathological Fracture: A break that occurs in a bone weakened by disease, such as osteoporosis or cancer.
3. Non-Weight Bearing (NWB)
Non-Weight Bearing (NWB) is a critical term in physical therapy, indicating that a patient should not place any weight on the affected limb or joint. This restriction is commonly prescribed following surgeries, fractures, or severe injuries to ensure proper healing without additional stress on the injured area.
When a patient is classified as NWB, they must avoid activities such as standing or walking on the affected limb. Instead, they rely on assistive devices like crutches, walkers, or wheelchairs to move around. The duration of NWB status depends on the severity of the injury and the specific medical recommendations of the healthcare provider.
Physical therapy during the NWB phase focuses on maintaining strength and flexibility in other parts of the body. Therapists may prescribe exercises that target the upper body and the non-affected lower extremities to prevent muscle atrophy and deconditioning. As healing progresses, patients may gradually transition from NWB to partial weight-bearing (PWB) and eventually to full weight-bearing (FWB) as tolerated.
4. Full Weight-Bearing (FWB)
Full Weight-Bearing (FWB) is a term used in physical therapy to indicate that a patient can place their full body weight on the affected limb without restrictions. This status is typically achieved after a period of non-weight-bearing (NWB) or partial weight-bearing (PWB) phases, which are necessary for healing after an injury or surgery.
Transition to FWB
The progression to FWB usually occurs after a period of rehabilitation, where the patient gradually increases the amount of weight they place on the affected limb. This transition is closely monitored by physical therapists to ensure that the limb can handle the stress without causing further injury.
Therapeutic Exercises
Once a patient is cleared for FWB, physical therapy focuses on exercises that improve strength, balance, and coordination. These exercises may include leg presses, squats, and functional activities like walking or climbing stairs. The goal is to restore the patient’s normal gait and functional ability.
Use of Assistive Devices
In some cases, patients may still use assistive devices such as crutches or a walker during the initial stages of FWB. As strength and confidence improve, these devices are gradually phased out.
Monitoring Progress
Physical therapists play a crucial role in assessing the patient’s progress during the FWB phase. They monitor for signs of discomfort, swelling, or instability, adjusting the rehabilitation plan as needed to ensure a safe return to full activity.
Importance in Rehabilitation
Achieving FWB is a significant milestone in the rehabilitation process. It indicates that the patient is nearing the end of their recovery journey and is ready to resume normal activities with minimal restrictions.
5. Home Exercise Program (HEP)
A Home Exercise Program (HEP) is a personalized set of exercises prescribed by physical therapists for patients to perform at home. The purpose of a HEP is to continue the therapeutic process outside of clinical sessions, promoting recovery, improving strength, flexibility, and mobility, and preventing the recurrence of injuries.
Customization
Every HEP is tailored to the individual needs of the patient. The exercises are selected based on the patient’s diagnosis, physical capabilities, and specific rehabilitation goals. This ensures that the program effectively addresses the patient’s condition and supports their recovery journey.
Types of Exercises
Exercises included in a HEP can vary widely, ranging from stretching and strengthening exercises to balance and coordination drills. Common exercises might include range of motion exercises, resistance training, and functional movements that mimic daily activities.
Frequency and Duration
The frequency and duration of the exercises are crucial components of a HEP. Physical therapists provide clear instructions on how often to perform each exercise, how many repetitions to complete, and how to progress the difficulty as strength and endurance improve.
Patient Compliance
Patient adherence to the HEP is essential for achieving the desired outcomes. Studies show that regular participation in a HEP significantly enhances recovery and reduces the likelihood of re-injury. To improve compliance, therapists often provide written instructions, videos, or digital platforms to guide patients through their exercises.
Monitoring and Adjustment
Physical therapists regularly monitor the patient’s progress with the HEP during follow-up appointments. Based on the patient’s feedback and progress, the program may be adjusted to introduce new exercises or increase the intensity to continue challenging the patient as they recover.
Importance in Long-Term Recovery
A well-designed HEP is crucial not only for short-term recovery but also for long-term health. By maintaining the exercise routine even after formal therapy ends, patients can sustain the improvements achieved during therapy and prevent future issues.
6. Physical Therapy (PT)
Physical Therapy (PT) is essential for restoring movement and function when someone is affected by injury, illness, or disability. It focuses on non-invasive treatments to help patients regain mobility, strength, and overall well-being.
- Assessment: The process begins with a detailed evaluation of strength, flexibility, and movement limitations to create a personalized treatment plan.
- Treatment Methods: Therapists use manual therapy, exercises, and modalities like heat and electrical stimulation to reduce pain and enhance recovery.
- Patient Education: Patients are guided on exercises and techniques to maintain progress at home, empowering them to manage their recovery independently. To enhance learning, healthcare providers can design and print posters online, creating visually engaging educational materials that help patients better understand their rehabilitation process and key exercises..
- Progress Monitoring: Continuous assessment and adjustment of the treatment plan ensure optimal recovery and adaptation to increasing physical demands.
- Goal: The primary aim is to improve the patient’s quality of life by restoring independence and functional abilities.
7. Passive Range of Motion (PROM)
Passive Range of Motion (PROM) involves the movement of a joint through its range by an external force, usually performed by a physical therapist or with the help of a device. Unlike Active Range of Motion (AROM), PROM does not require the patient to exert any muscle effort.
- Purpose: PROM is crucial in early rehabilitation stages, especially when patients are unable to move a joint themselves due to pain, injury, or surgery. It helps maintain joint flexibility, prevents stiffness, and promotes circulation.
- Application: Therapists often use PROM to gently move the affected joint through its full range to keep the muscles and joints supple. This technique is especially important for patients with severe injuries, neurological conditions, or post-operative recovery.
- Benefits: Regular PROM exercises can prevent muscle contractures and joint deformities, reduce pain, and improve circulation, aiding in faster recovery and overall mobility.
- Therapist’s Role: The therapist carefully monitors the patient’s response to PROM exercises, ensuring that the movements are performed within a pain-free range and adjusted as the patient’s condition improves.
8. Active Range of Motion (AROM)
Active Range of Motion (AROM) refers to the movement of a joint that is accomplished by the patient’s own muscle power. It is a critical aspect of rehabilitation and recovery in physical therapy, allowing therapists to assess and improve the functional capacity of a patient’s joints and muscles.
- Purpose: AROM exercises are designed to enhance muscle strength, coordination, and flexibility. These exercises are typically introduced after Passive Range of Motion (PROM) exercises once the patient is able to actively engage the muscles around the joint.
- Application: Patients perform AROM exercises independently, moving their joints through the full range of motion without assistance. These exercises are crucial for building muscle strength, improving joint stability, and restoring functional movement patterns.
- Benefits: AROM promotes muscle activation, enhances circulation, and helps prevent muscle atrophy. It also aids in increasing joint mobility and preparing patients for more demanding physical activities.
- Therapist’s Role: The therapist guides the patient on how to correctly perform AROM exercises, ensuring proper technique and safety. They monitor progress and adjust the difficulty of exercises as the patient gains strength and mobility.
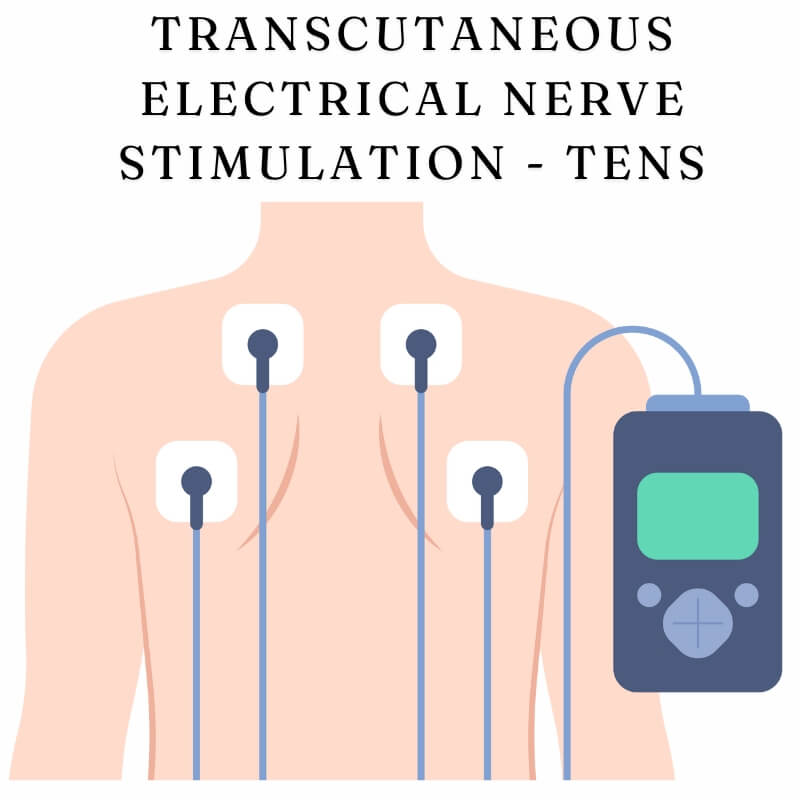
9. Transcutaneous Electrical Nerve Stimulation (TENS)
Transcutaneous Electrical Nerve Stimulation (TENS) is a therapeutic modality used in physical therapy to relieve pain. It involves the use of a small device that delivers low-voltage electrical currents through electrodes placed on the skin near the affected area.
- Purpose: TENS is primarily used for pain management. The electrical impulses help block pain signals from reaching the brain and stimulate the production of endorphins, the body’s natural painkillers.
- Application: TENS can be used for a variety of conditions, including chronic pain, post-operative pain, and acute injuries. It is commonly applied to areas such as the back, neck, and joints. The intensity and frequency of the electrical impulses can be adjusted depending on the patient’s needs and tolerance.
- Benefits: TENS provides non-invasive pain relief, reducing the need for medications. It is a versatile treatment option that can be used in both clinical settings and at home with proper guidance from a therapist.
- Therapist’s Role: The therapist determines the appropriate settings for the TENS device and teaches the patient how to use it safely and effectively. They may also integrate TENS with other therapeutic interventions to enhance overall treatment outcomes.
10.Activities of Daily Living (ADL)
Activities of Daily Living (ADL) refer to the routine activities that people perform every day without assistance. In physical therapy, ADLs are a key focus, as they represent essential functions that contribute to an individual’s independence and quality of life.
- Purpose: The primary goal of physical therapy is to restore or improve a patient’s ability to perform ADLs independently. These activities include basic tasks such as eating, bathing, dressing, grooming, and mobility.
- Application: Physical therapists assess a patient’s ability to perform ADLs and develop a rehabilitation plan to address any deficits. Therapy may involve strength training, balance exercises, coordination drills, and functional mobility tasks. The exercises are often tailored to mimic the specific ADLs that the patient struggles with.
- Benefits: By focusing on ADLs, therapy helps patients regain independence, reduces the need for caregiver support, and improves overall quality of life. Successful ADL rehabilitation can also prevent further physical decline and contribute to better mental health by enhancing self-esteem and confidence.
- Therapist’s Role: Therapists play a crucial role in teaching patients how to safely and effectively perform ADLs, often providing adaptive strategies or assistive devices to aid in the process. Continuous monitoring and adjustments ensure that the patient makes progress towards regaining full independence.
FAQs
What is the difference between Passive Range of Motion (PROM) and Active Range of Motion (AROM)?
PROM involves the therapist moving the patient’s joint through its range without any effort from the patient, while AROM requires the patient to actively use their muscles to move the joint. PROM is often used when the patient is unable to move the joint themselves, while AROM is used to assess and improve muscle strength and joint function.
How long should I use a TENS unit each day?
The typical duration for using a TENS unit is about 20 to 30 minutes per session, up to three times a day. However, the exact time can vary depending on the specific condition being treated and the recommendations of your therapist. Always follow the guidance of your healthcare provider for safe and effective use.
Can a Home Exercise Program (HEP) replace regular physical therapy sessions?
A HEP is designed to complement regular physical therapy sessions, not replace them. It allows patients to continue their progress between sessions, but regular in-person therapy is often necessary for monitoring, adjusting treatment plans, and providing hands-on care that can’t be done at home.
Is it normal to feel pain during Active Range of Motion (AROM) exercises?
Mild discomfort during AROM exercises can be normal, especially if you’re recovering from an injury or surgery. However, you should not feel sharp pain. If you do, it’s important to stop the exercise and consult your therapist, as it may indicate that the exercise is too intense or being performed incorrectly.
What types of fractures require the most physical therapy?
Complex fractures, such as comminuted fractures (where the bone is broken into several pieces) or compound fractures (where the bone pierces the skin), generally require extensive physical therapy. These types of fractures often involve longer immobilization periods and more significant muscle atrophy, necessitating a comprehensive rehabilitation plan to restore full function.
Can I use a TENS unit on any part of my body?
TENS units can be used on many parts of the body, but there are certain areas to avoid, such as directly over the heart, on the front of the neck, or on broken or irritated skin. It’s essential to follow the instructions provided by your therapist to ensure safe use.
Last Words
These terms help streamline communication between patients and therapists, making treatment more efficient and effective. By familiarizing yourself with these abbreviations, you can take an active role in your recovery, ensuring that you and your healthcare provider are on the same page.